A team of researchers at Massachusetts Institute of Technology (MIT) has been refining and combining several advanced technologies over the past six years to create a revolutionary platform to treat a vast array of neurological diseases and mental illnesses. It could not only prove more effective than traditional methods, but also negate the need for complex procedures that carry their own set of risks.
It’s called Circulatronics, and the idea is to use a fusion of electronics and biological transport to autonomously implant bioelectronics within the body – completely avoiding the need for surgery to enable modern forms of treatment.
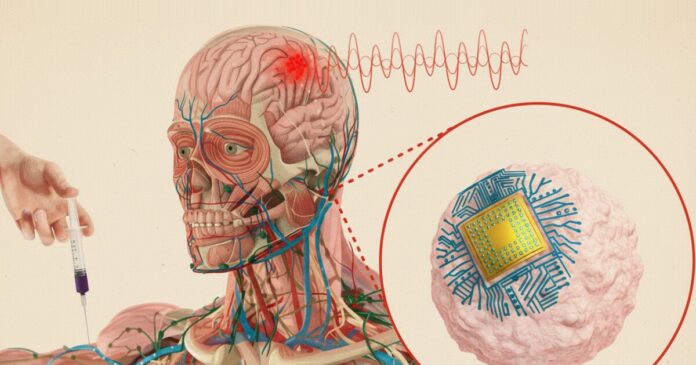
The tech is centered around using targeted electrical stimulation aimed at the brain for various conditions. In recent years, this approach has been applied to treating depression, Alzheimer’s disease, Multiple sclerosis, and brain tumors.
Normally, you’d have to undergo invasive surgery to embed electrodes into your brain for this – a procedure that introduces the risk of infection and possible damage to brain tissue. These surgeries are also expensive and hard for most of the 3 billion people with neurological disorders worldwide to access.
The integrated technology does away with this entirely. Instead, it involves sub-cellular sized wireless electronic devices (SWED) that can be delivered to your brain via a jab in the arm. Once these tiny chips have been injected, they can autonomously implant themselves on target regions in the brain, and power themselves as they deliver electrical stimulation to the affected areas.
Surgery-Free Brain Implant for Brain-Computer Symbiosis
Circulatronics has been described in a paper that appeared in Nature Biotechnology last week; senior author Deblina Sarkar heads the Nano-Cybernetic Biotrek Lab at MIT, and she collaborated on the work with other researchers from MIT, Wellesley College, and Harvard University. You can watch her explain the technology in the video above.
There are two fascinating aspects to this technology: the SWEDs themselves, and the way they reach your brain.
First off, the core electronics are truly small, measuring about one-billionth the length of a grain of rice. They’re made of organic semiconducting polymer layers sandwiched between metallic layers to form tiny chips, and they’re compact enough to fit on a circulating blood cell. The SWEDs are designed to harvest energy wirelessly using the photovoltaic principle, i.e., converting light into electricity. This means they can be powered by applying light from outside the body, such as a near-Infrared laser that can pass through the skull.
Image courtesy of the researchers
These devices allow for highly focused stimulation of deep brain areas with remarkable accuracy. And even at this miniature scale, the devices can generate nanowatts of power to zap the brain with tiny jolts of electricity.
To guide these SWEDs to the brain, they’re fused with living immune cells called monocytes to create a cell–electronics hybrid. These cells are able to safely cross the blood–brain barrier, and they naturally seek out and travel to regions of inflammation in the body. Inflammation is a known therapeutic target for many neurological diseases, so these hybrids find their way to those areas of the brain and self-implant there.
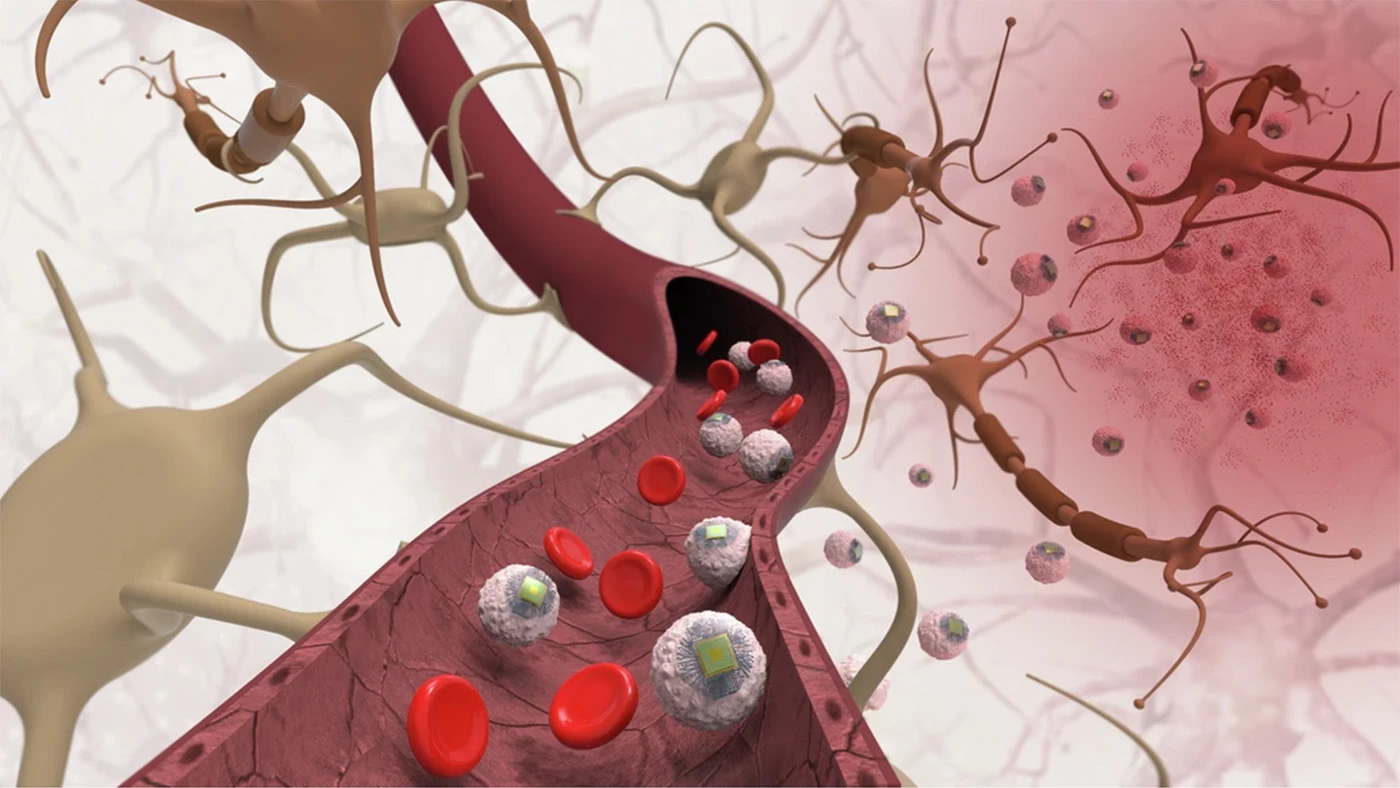
Image courtesy of the researchers
Once the hybrid is implanted at the target site, the SWED can be activated wirelessly by shining a laser from outside the body. This triggers the electrical stimulation needed for specifically adjusting the activity of neurons in a very small, targeted area of the brain (which is called focal neuromodulation).
This technology was tested in two phases using mice to make sure the concept – using cells to deliver and run brain implants without surgery – is safe and effective.
To prove this self-guided delivery system works, researchers first created a small, inflamed area in a deep brain region of mice. This was done to simulate a diseased spot that the cells would naturally seek out (like inflammation caused by Alzheimer’s, or a stroke). The hybrids were injected directly into the mice’s bloodstreams. After 72 hours of waiting to allow the cells time to travel and self-implant, the team found a large number of the experimental electronics successfully landed right at the target location.
Next, the mice with the successfully self-implanted hybrids were subjected to wireless optical stimulation using a near-Infrared laser. Researchers looked for c-Fos, a protein that serves as a marker for newly active brain cells, to see if the stimulation worked. They found that the mice with implanted hybrids showed a high number of activated c-Fos-positive brain cells. Not only that, the activation was highly focused, within just 30 µm of the inflamed region.
That could make next-gen treatments available to far more people in the years to come, and make it more feasible to expand access to regions where brain surgery is hard to come by. Sarkar and her team are developing Circulatronics further to treat brain cancer, Alzheimer’s disease, chronic pain, and other conditions. They’re also exploring ways to add more nanoelectronic circuits into their SWEDs to enable sensing and even creating synthetic electronic neurons.
We might also see this tech go beyond treating neurological conditions. “This technology is not just confined to the brain but could also be extended to other parts of the body in future,” Sarkar noted. It can be directed towards other organs, and even help deploy devices like wireless pacemakers.
When will this arrive at a hospital near you? Through an MIT spinoff startup called Cahira Technologies, Sarkar is working to get Circulatronics into clinical trials within three years. It will go through several more years of approval procedures before it can be made commercially available. So yes, it’s going to be a while, but it could indeed play a huge role in the future of medical care.
Source: MIT