When an ulcer creates an actual perforation in the digestive tract, surgery is currently the only treatment. In the not-too-distant future, however, such holes may be easily plugged with the equivalent of a tiny remote-control swallowable pen.
Currently in prototype form, the “pill-sized” MEDS (Magnetic Endoluminal Deposition System) is being developed by Vivek Subramanian, Sanjay Manoharan and colleagues at Switzerland’s EPFL research institute.
Its pen/syringe-like body is filled with a bio-ink made up of seaweed-derived sodium alginate gel and live human gastric fibroblasts. The latter are the cells which form the stomach’s connective tissue.
Located directly behind the load of bio-ink is a spring-loaded plunger, held back by a stopper made of PLA (polylactic acid) polymer. Located in front of the bio-ink – at the “dispensing” end of the gadget – is a nozzle consisting of a gold-coated neodymium-iron–boron ring magnet.
EPFL
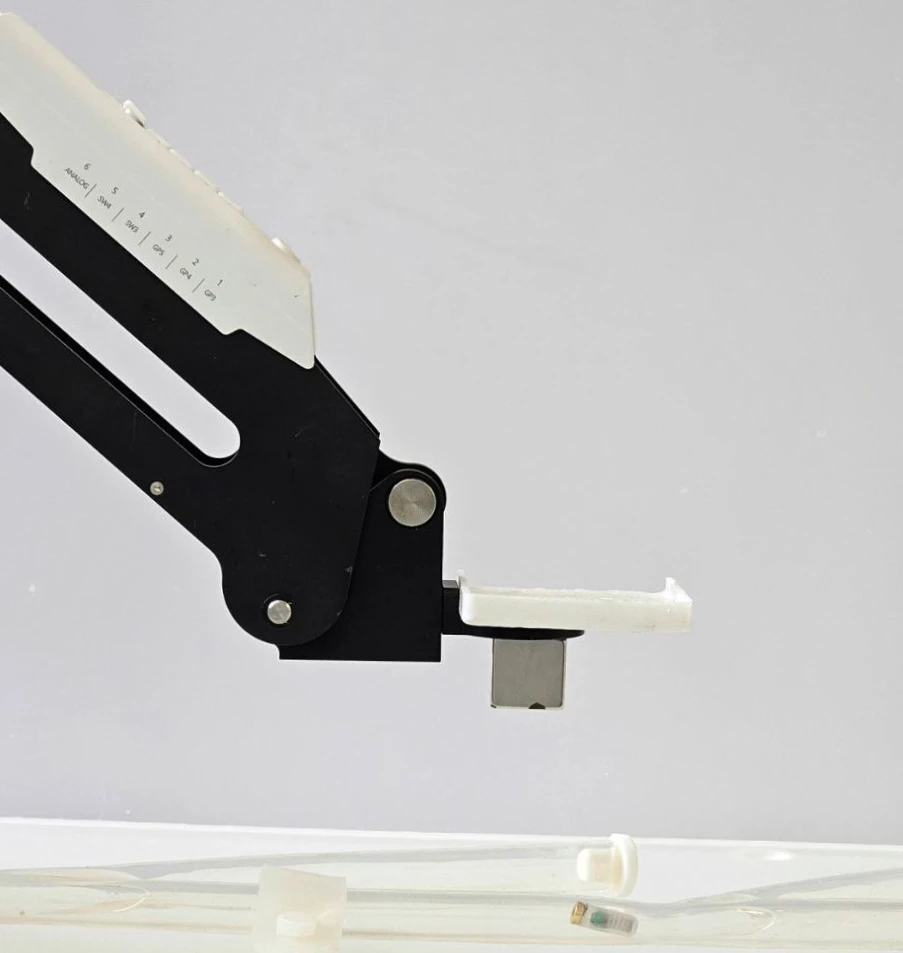
After MEDS has been swallowed by the patient, a magnet on a robotic arm is used to externally guide the magnet-bearing device through the digestive tract, to the site of the ulcer. Medical imaging is utilized to facilitate this process.
Once MEDS’ nozzle is in place against the ulcer, a near-infrared light (NIR) source is placed against the skin on the outside of the body, emitting light through the tissue. The heat energy in that light causes the PLA stopper in MEDS to melt, thus releasing the plunger and allowing it to push the bio-ink out of the nozzle.
Not only does the bio-ink plug the hole, but as the fibroblasts grow and reproduce, the ulcer should actually heal. The technology has already been used to treat artificial ulcers on simulated gastric tissue, and to deposit the bio-ink in the digestive tracts of rabbits who did not have ulcers. Instead of being passed with the feces after use, the MEDS devices were guided back up out of the animals’ mouths.
EPFL
“In our controlled lab experiments, our cell-laden bio-ink retained its structural integrity for over 16 days, suggesting its potential as a ‘micro-bioreactor’ that can release growth factors and recruit new cells for wound healing,” says Sanjay Manoharan, who is a PhD student in Vivek Subramanian’s lab.
A paper on the research was recently published in the journal Advanced Science.
Source: EPFL


